-.-. .- .-. . –. .. …- .. -. –.
This is Morse Code for “caregiving”. If you don’t know how to break the code, you’ll be left scratching your head as to what the dots and dashes mean. Another code, of sorts, exists behind the term “caregiving” itself as not everybody can completely explain this role or even properly define the word. This is likely because there are various types and levels of caregivers and many people don’t readily identify themselves as caregivers at all!
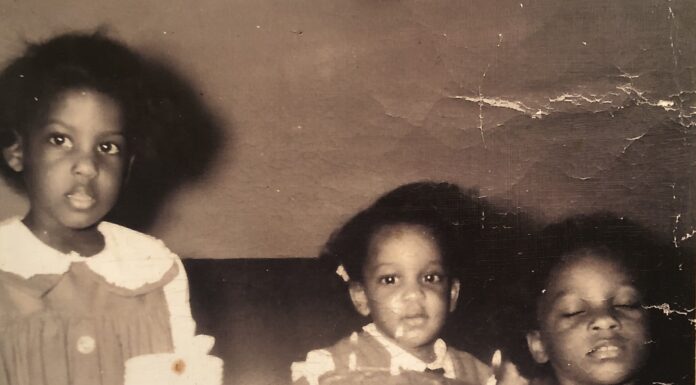
When one hears the term, “caregiver”, the picture that often springs to mind first is that of an adult child caring for an aging parent … perhaps a son or daughter pushing Mom / Dad around in a wheelchair. With more than 44 million individuals in the US serving as informal and unpaid caregivers (AARP, 2004), it’s easy to understand why this common mental image exists. This is, in fact, my own experience as I helped and supported both my mother and father before they passed away – a job which could have been far more burdensome without my two sisters. And with our country’s aging population, more and more family members will be certainly assuming numerous responsibilities for their own parents. But a caregiver can really be anybody providing assistance to another individual – whether this be a friend, partner or spouse. Care recipients don’t have to be old or even human either! Parents of disabled children can also be considered caregivers. More and more senior’s residences are recognizing the value of family pets as caregivers through pet therapy programs – a dog or cat visiting a senior can serve to calm, provide enjoyment and increase the quality of life for these people.
Confusion can also exist between the terms “informal caregiver” and “formal caregiver”. The first group are, typically, untrained and unpaid family members. They will be lucky to have any related experience (e.g. healthcare, legal, social work or finance) and can be bewildered and overwhelmed with the job. “Formal” caregivers are, on the other hand, trained and paid professionals (doctors, nurses, social workers, physiotherapists, etc.). They will often play key roles on one’s own caregiving team and have a much better idea of medical conditions, how to administer the best care possible and how better to navigate the often-puzzling “system” to find required assistance.
Another unclear term can be the “sandwich generation caregiver”. This person is caught in the middle between their own younger children and aging parents. Obviously, this will demand more of a caregiver’s time and energy, so a sandwich generation caregiver should be much more mindful of his/her amount of work conducted for both sides of his/her family so as to avoid excessive stress. Taking this analogy further, there is also the “club sandwich generation caregiver” (an individual with young children, aging parents and grandparents).
Further misperceptions may occur when considering the type of care provided (which can take many different forms). Caregivers can provide hands-on care (e.g. bathing, clothing, medication delivery, etc.); however, this physical assistance may be best left to properly trained and/or experienced healthcare workers who will know the best procedures. Trying to lift, transfer, bathe or clothe a senior independently if you are not sure of the proper methods and may not be completely comfortable with doing so can prove to be dangerous (for both the caregiver and the care recipient). Other care options can include visiting a senior to play cards, driving a senior to a day program, having bank signing authority granted and paying a senior’s bills, helping with house cleaning, separating prescription pills into daily dispensers, helping a senior eat a meal, serving as a Guardian or Trustee and so on. Two aspects of my own caregiving role with my father before he passed away were accompanying him on regular walks to help increase his fitness and flexibility and reading to him in hopes of keeping his mind active for as long possible. Help provided can come on either a large or small scale. Whatever the caregiver can comfortably do can be greatly appreciated.
On a final note, it is interesting when caregivers may not immediately identify themselves as caregivers. I believe this could be for many reasons: unfamiliarity with the term, shame, embarrassment, denial or refusal to accept outside help (this is my parent and therefore he/she is my responsibility …). Without identifying yourself as a caregiver, however, may lead to isolation (on your part and others who may be caregivers themselves who don’t know where to turn). In fact, the more often you speak up as a caregiver, the more likely it will be for others to listen and provide answers for you – whether this would be developing a new senior’s respite program in your area so you can take a much-needed break; recommending a specific type of grab bar to install in a senior’s bathroom to make it safer or lobbying politicians for increased caregiving funding and support at local, provincial and national levels.
With time, patience, knowledge and skill, there is no code that cannot be broken and the caregiving code is no different. Unlocking the mystery behind caregiving is one of the first important steps to better understanding your forthcoming or newfound role and better understanding how you can best provide help.