Given the risk of chronic disease increases for all of us as we age, it’s not surprising that two out of three older Americans have multiple chronic conditions. These conditions often involve complex treatments, like juggling a handful of different medications. That’s why we put together this toolkit. This medication management guide will empower seniors, caregivers, and family members with helpful information about medication use, storage, organization, and more.
In this guide, you’ll learn how age changes our response to medication, and how to keep track of the medication you’re taking. You can also find out how you can reduce your medication error and drug interaction risks.
Throughout this guide, you’ll find tips for becoming a more active part of your own health care. We believe education empowers you. Of course, it’s important to always check with your doctor or pharmacist before you take any new medication or make changes to your medication regimen, so be sure to ask your healthcare provider how the information in this guidebook can apply to your individual health.
Effective medication management requires teamwork
You’re an important part of your own health care—which is why you should educate yourself and be an empowered consumer. To be successful, you’ll need to partner with your healthcare team to keep them informed and work together to make the right medication adjustments. Instead of prescribing medication once and refilling it for the rest of your life, your doctor needs to be aware of health status changes that may affect or even eliminate your need for certain medications altogether.
“I would also recommend asking if there are any medications which are no longer needed,” says Erin Pitkethly, pharmacist at Robinsong Health Low Carb Clinic. “It is very common for meds to be added on, but it is uncommon for them to be stopped even when they are no longer needed. ”
Adding to the potential confusion, many seniors have a mix of different medicines, some of which are prescription and some that are not. Even if it’s just a medicine you take for a temporary condition, it’s important to read labels and understand why you’re taking every drug.
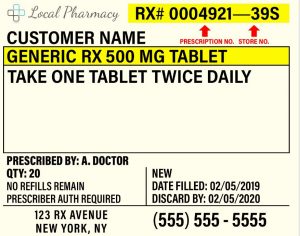
Regardless of the type of medication, it should have a label with basic information that can serve as your guide and starting point.
Reading medication labels
As you review your new prescription, be sure to read the label carefully for information on dosage, timing, interactions, and other important medication management details.
Typically, a prescription label has eight parts and types of information. Keep in mind that your own prescription labels may look somewhat different, but they will generally have similar content listed for you to reference. Learn to recognize these parts on your own medications:
- Pharmacy information: Name and address, phone number, and other key details about the pharmacy that filled your prescription.
- Your information: Name and address of the person the drug is prescribed to.
- Prescribing doctor’s information: Physician or healthcare provider’s name and contact information are also included.
- Drug name and strength: Medicine’s brand, chemical, or generic name along with the strength of one unit of the prescription in a measurement such as milligrams (mg).
- Instructions: Instructions might read “Take one tablet twice daily, morning and night, by mouth” and explain how and when to take the medication. Always read the instructions section carefully for any new medication, and ask your doctor or pharmacist if you have questions.
- Prescription information: Date your medication was prescribed, the date your medication was filled by a pharmacist, the number of pills or doses provided, how many times your prescription may be refilled, when your medication expires, and the number your pharmacy assigned to your prescription.
- Pharmaceutical manufacturer information: Name of the company that manufactured your medication and a physical description of the drug. If it’s a generic version of a brand-name drug, the name of the branded counterpart may also be listed here.
- Federal caution statement: Prescription warnings such as “Caution: Federal law prohibits transfer of this drug to any person other than the patient for whom prescribed.” Remember, you should never take someone else’s medication even if you’ve taken it before. It’s dangerous to take medicine that’s not prescribed for you and doing so could put your health at serious risk.
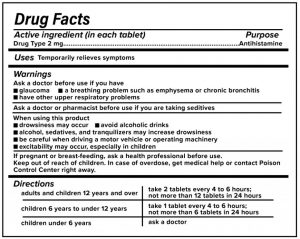
An over-the-counter medication you can purchase without a prescription has a different label, called a drug facts label. Here’s what that usually includes according to U.S. Food and Drug Administration (FDA) regulations.
- Active ingredient(s): The therapeutic ingredients within your medication and the amount in each dose.
- Uses: Any symptoms or condition the medicine is designed to treat or prevent.
- Warnings: This section tells you when you shouldn’t use this medicine, lists possible side effects and drug interactions, lists any conditions that may require a doctor’s advice before taking the medicine, tells you when you should stop taking the medicine and see a doctor, and provides other critically important information about taking the medication. Read this section carefully. If you’re concerned about anything you see, talk to a healthcare professional.
- Inactive ingredients: Other substances added that don’t have a therapeutic effect, such as colors or flavors.
- Purpose: The medicine’s category or action is included (for instance, antacid or pain reliever).
- Directions: Dosage information may offer different doses for different ages or symptoms. It may also direct you to ask a doctor.
- Other information: Anything else the manufacturer wants you to know about the medicine. It may include information about how to store the drug. It may also list how much of an ingredient (such as calcium) the medication contains.
When you get a new medication, take a look at the label and jot down any questions you have for your healthcare provider. If you’re using medication reminders, add this prescription so everything is ready for the first day of treatment. If you encounter anything unusual or confusing on your label, check with your pharmacist.
Do keep in mind that your prescription is tailored to your health. Even if a friend or family member is taking the same medicine, your medication may work differently for you. This is one reason why it’s absolutely essential to refer to your healthcare team for medical advice and information instead of other sources (like the internet) meant for a broad audience. Only your healthcare provider can give you relevant guidance for how to take medications safely.
Aging changes our responses to medication
As we age, our bodies change how they interact with medications. Even very healthy people might respond differently to medications than they did in earlier years. Getting the most from your medications is possible with close cooperation with your healthcare team.
How does aging change the body’s reaction to pharmaceuticals? Here are few possible changes.
- Metabolism: Your body processes each medication at a different rate. Over time, your metabolism of a particular drug may speed up or slow down. This can increase the risk of side effects or decrease the effectiveness of the drug.
- Brain and nervous system: Many drugs impact the central nervous system (CNS) directly and aging can change this process. For example, seniors are more susceptible to the CNS effects of drugs like benzodiazepines and antidepressants.These effects can include increased dizziness or drowsiness for some people.
- Kidney and liver function: Since these organs are responsible for filtering and cleaning, any age-related changes to kidney and liver function can adjust how well your body is able to remove medicines and toxins.
- Weight changes: Many people gain or lose weight as they experience appetite changes. Some drugs are processed and distributed differently throughout the body depending on your body weight.
“Elders have less tolerance for medications than younger adults,” says Elizabeth Landsverk, MD, a board-certified geriatric doctor and founder of ElderConsult Geriatric Medicine. Dr. Landsverk notes that these changes in how our bodies process medication can lead to different side effects. The timing of new side effects may provide clues to the root cause, however. “If a symptom starts after a new medication, it’s likely a side effect from the new meds,” she says. “Seek the advice of a doctor or pharmacist, they will likely change the prescription. Do not change dosages or try a different medication based on something you read on the internet.”
Aging may also change the dosage you need before your medications are effective. So your healthcare providers should regularly reevaluate the medicines you’re taking to see if new prescriptions are necessary. According to Dr. Landsverk, many seniors gradually lose their appetite and experience weight loss that impacts medication dosage.
If you notice anything different or unusual during treatment, it’s important to bring this up during your next conversation with your doctor or pharmacist.
Medication safety tips and dosage information
Knowing how to manage your medications can be the key to benefiting the most from your treatments. Medicines have the potential to make life-changing improvements to your health. At the same time, your medications are only helpful if you know how to use them correctly.
Ultimately, your doctor or personal healthcare provider and your pharmacist should be your guide on how to use and track your medications. When in doubt, be sure to check with a qualified health professional. Only your healthcare provider or pharmacist knows how your individual health profile, health status, and history impact your medication needs.
Medication safety also means knowing where many seniors go wrong with medication management and how you can avoid those mistakes to protect yourself.
Common medication mistakes and how to avoid them
“The two key challenges that seniors face are polypharmacy (taking lots of pills) and remembering to take them,” says Dr. Ceppie Merry, who holds a Ph.D. in pharmacology. “It can be really complex to remember what to take and when to take them.” Merry also adds that any cognitive decline or complex conditions seniors have can make it even easier to make mistakes when managing your own medications.
Medication errors can have serious consequences for your health. Many people accidentally take the wrong dose, miss doses, or take their medications incorrectly. Don’t panic if you use your medication incorrectly, but do call your doctor if you’re concerned. (If you are experiencing a life-threatening emergency, call 911.) The adage “better safe than sorry” applies here. This is why you should always keep important phone numbers like your doctor’s contact information nearby in case you need to call their office.
To stay on track with taking your medicines, it helps to have a medication strategy. Here’s what you can do to reduce your risk of a serious medication error.
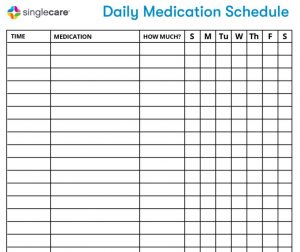
- Take medications consistently: Always take your medications at a consistent time. It also helps with consistency if you can associate taking the medication with a specific event like a meal. For instance, if you take a pill with breakfast at 8 a.m. one day, try to always take that medicine around 8 a.m. when you eat.
Download the Daily Medication Schedule
- Use reminders: Forgetful about taking your medicine? Consider using a reminder app or setting an alarm for each dose.
- Prevent interactions: Many medicines can’t be taken together or with specific foods or supplements. A lot of medications interact with citrus fruits, for example. Your pharmacist can help you identify any diet or medication list changes you need to make.
- Get a medication review: With every new prescription, ask your pharmacist to review your medication and supplement list. Your healthcare provider may recommend ideas for how to take them together safely. Also, see if you’re eligible for your pharmacy’s medication therapy management (MTM) program. Your pharmacist will sit down with you for a comprehensive medication review at no additional cost to you.
- Ask your doctor or pharmacist: If you’re prone to forgetting doses or taking an extra pill now and then, ask your healthcare professional what you should do if this happens. Sometimes, it’s not a big deal. Other medications might cause a serious interaction, side effect, or other serious damage to your health.
- Read the literature and instructions: If your medication came with written information or your healthcare provider included instructions, be sure to read these carefully. If anything is unclear, don’t hesitate to make a note of it. Call your doctor and ask for clarification before you start taking your medication. It’s a good practice to read the instructions before you leave the pharmacy, so you can ask the pharmacist.
Have trouble remembering your medications? Here are a few ideas to try.
- Use a dosage reminder or pill reminder app: Consider using a smartphone pill reminder app to remind you to take medication.
- Set an alarm: Set an alarm for times during the day that you take your medicine. Be sure to keep track of what you’re supposed to take, too.
- Make a list: Write down a list of your medicines and the time you take them so you can easily refer back to it later.
- Ask for help remembering: If a family member, friend, or caregiver can help you remember, ask for their help.
- Add it to your calendar or planner: Write down reminders in your calendar or planner.
- Use sticky notes, send yourself emails, or post other reminders: Think about how you manage your time and how you use reminders. Choose a method that works best for you.
- Use a pill organizer for medication storage: At most drugstores, you can buy an inexpensive pill organizer with compartments for different times and days. This works best if you take a small number of medications every day.
Keeping your medications organized may also prevent mistakes. Here’s how to get started with tracking and organizing medicines.
Organizing your medications and medication storage
Managing your medications is easier when you can fully account for everything you’re taking. With the help of a healthcare professional (if needed), gather all the medications and supplements you’re currently taking and start organizing them.
Consider these tips to help with medication management.
- Create a medication list (if needed, use a medication list template): Write the name of each prescription you’re taking on the list. You can also add information about how often you take each dose and for what condition, but the important thing is to start with a complete list of drug names and doses so your healthcare provider knows where to look and what questions to ask.
- Start with supplements: Since so many people don’t consider supplements to be medications, it’s not uncommon for some seniors to take supplements that interact with medications prescribed by their doctors (or contain unhealthy ingredients). Bottom line—your doctor needs to know. Make sure your personal medication list template covers supplements.
- List all OTC (over-the-counter) medicines you take: Many seniors take drugstore medications that are sold over-the-counter without a prescription such as acetaminophen (the generic version of Tylenol) for pain relief or calcium carbonate antacids for managing heartburn.
- Keep medication packaging: Hold onto the original boxes and containers for your medications so you can quickly refer to the package or label if needed. Package inserts or patient information leaflets are included with the medication so be sure to keep it with the original packaging. A shoebox-size plastic storage bin with a lid or a gallon-size plastic bag are great ways to store packaging and information for medicines you’re currently taking. Always store your medicines and packaging away from where pets and children can reach them, even if your medicines have child-proof caps.
- Pick one pharmacy: Ideally, you should only use one pharmacy so your pharmacist can easily review your other prescriptions and provide you with relevant information about contraindications. If you must use more than one pharmacy for any reason, be sure to provide complete information about the medications you’re currently taking, and make sure the pharmacist has access to this information.
As you organize your medications, don’t forget to check expiration dates and remove medicines you no longer take. Ask your doctor if it’s okay to discard old medication documentation.
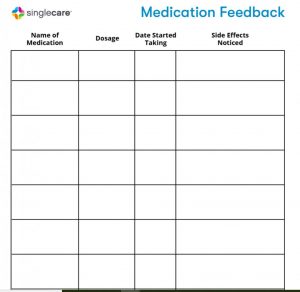
Reviewing medicine with your pharmacist or doctor
Periodically, you should have a medication review appointment with your doctor. During these appointments, you’ll want to keep your doctor informed about how your treatment is going. This is also a good time to ask questions and express your concerns. Highlight any side effect you haven’t told your doctor about yet, and mention any frustrations or concerns you have with your medicines. Don’t forget to bring a list of questions with you. Since many doctor appointments are short, make the most of your time together by preparing a list of topics and questions beforehand.
Download the Medication Feedback Form
By educating yourself and managing your medications properly, you may get better results from your treatment and you may avoid some of the common risks of using medicines. Your healthcare team is there to help you. Work closely with them and become your own healthcare advocate.