As a former mental health and substance abuse therapist, it was easy to see that many of my clients were using or used some form of illegal or controlled substances or alcohol to hide from unwanted memories. Crack cocaine was the drug I once used to blur my abuse. Memories of traumas change a person’s soul and their view of the world. We create our reality by our life experiences, good, bad, or indifferent.
Those involved in helping create suffering in others’ lives are frequently people we should have trust in and usually have little to no concern about the consequences of their inflicted on others.
At times the difference between victim and perpetrator is a fragile line, then some struggle to see victim or perpetrator for one reason or another. Many times, it is the personal relationship between one or both that tends to skews perception.
Victims, a person harmed, injured, physically or mentally, or killed by abuse or neglect are of all ages, sexual orientations, races, and nationalities. The perpetrator, a person who causes distress, torment, or wrongdoing, is also not defined by age, sexual orientation, race, and ethnicity.
My Story –
October 10, 2019 – I received a call from the parent of a client who lived three hours away from my home office after 5:00 p.m. I would not get to my client’s home until around 7:00 p.m., Nashville time. Darkness would fall by the time I arrived. The mother stated that her daughter was in crisis and needed me to drive to Nashville due to the violent history of assault. The home had confederate flags inside and out. To say the least, I was uncomfortable in this home.
From day one, I stressed my concern about my company willing to send a person of color into this home. I voiced my opinion several times to my supervisor, who was unwilling to rethink services for this client’s home. Her comments to my expressed concerns, “Oh fun,” not once but all three times, during prior visits to this home.
Once I reached the home to help with the crisis, I quickly realized there was no actual crisis. Things felt off during the visit, and once I did my part and was about to leave, all hell broke loose. Before I knew it, I was being assaulted and thrown to the floor. My client was hitting, kicking, pulling my hair, growling, and trying to bite me. What many are unaware of is that mentally ill clients seem to have the strength of superman. I’ve worked with six-year-old children who required no less than five adults to hold and subdue them for as long as twenty minutes at a time. House staff has been brutally assaulted by frail-looking, mentally ill seniors as well.
This assault went on for about ten minutes as the mother and sister watched. As I yelled out for the mother to call 911, she did nothing and sat in her front-row seat watching the attack. All she needed while watching the action was a soda and popcorn. When she did get up, it was only to watch the assault from a different view. My client and I rolled around on the floor as I tried to avoid her attempts to bite me. It was as if we were glued together in a spinning tornado. After seventeen years working in mental health, this was the first time a client ever attacked me.
Each time I thought I had a chance to get away from the client, she quickly pounced like a cat on a rat, scratching, clawing while making hideous howls and growls. With one hand violently pulling at my hair, the other was trying to scratch off my skin. When we were not rolling on the floor, her long skinny legs kicked at my stomach like a boxing kangaroo. All of this as her mother watched with her cellphone in her hand. The mother did not attempt to stop the assault on me.
Once I could free myself from the maniacal kicks, throws, and blows of my client, I grabbed my phone and went outside to call the police. Within minutes the fire department, the EMS, and the police had arrived. Nearly everyone who responded to my call was familiar with this client and her attacks on others, including medical staff and the law. Once I provided the needed information, my client was removed from the home and taken to a hospital. She would spend several months in no less than two psychiatric hospitals after this incident.
After the attack, I pleaded with my supervisor that I was still leery about returning to the home, and we should drop this family from our services. My supervisor responded by saying that we still had to provide services to this family, and unfortunately, there were no white coordinators available to go work with this family. Fortunately, my client’s lengthy hospitalizations kept us apart, and once Covid-19 started, my agency stopped home visits in early March. To this day, I still hear the client’s growls.
January 23, 2020 – During a routine visit with another client who also had a violent history of attacking people, I became the witness to his brutal attack on his mother. Two weeks prior, I saw this client attack his mother twice in one day.
I witnessed both attacks on the same day while at a meeting. I again warned my supervisor and TennCare insurance about my apprehension visiting this home during a phone conversation. I stated the son would eventually attack or try to kill his mother, and I would be the unfortunate one to be there when it happened. The day I said this was the day it happened, and I was there.
After this conversation, I went into the home to discuss plans for my client with his mother. Within minutes he became erratic and difficult to redirect. I immediately knew something terrible was about to happen. Before I could intervene, my client flew through the air, and purposely landed on top of his mother as she sat on the couch. My client’s mother started screaming, “Help me; help me.” Her son started growling and pounding her with both fists. When he was not punching her, he was pulling her hair out. She began to bleed.
I tried to pull the client off of his mother. It felt as if I was trying to pull a redwood tree out of the ground by its roots. He continued to hammer his mother as her screams turned into cries. I yelled out the client’s name telling him to get off of his mother. For a few seconds, my client’s fists stopped in midair, and he looked at me. His mother’s crying stopped as she gasped for a breath. Then my client went back to punching her.
I grabbed my cellphone and called 911. As I reported the incident, my client kept assaulting his mother, and his mother kept crying. The officer talking to me could hear her terrifying screams. Within a few minutes, eight police officers had arrived, ending the assault. The mother, who was still bleeding, refused to go to the hospital. Her son, however, did. I would never forget the look on this mother’s face or her screams during the beating, ever.
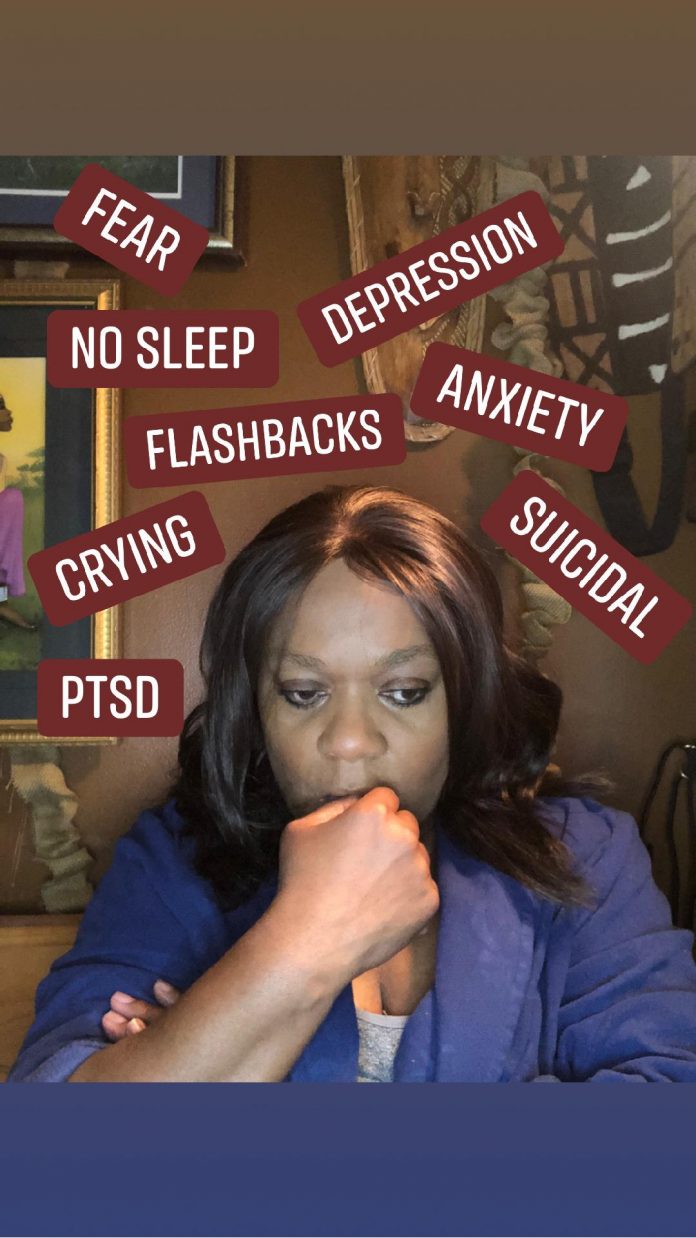
April 2020 – After months of attempting to put both attacks behind me, I could no longer put off the physical and mental issues that developed as a victim and witness to both assaults. I could not get the visuals of what happened to me, what I saw, or the looks of everyone’s face involved out of my head. I was reliving both assaults like a repeating movie. PTSD does not always start immediately after a traumatic incident. Once I was sure that I was dealing with it, I reached out for help. I needed help and began seeing a psychologist through a company related short term program until a long-term psychologist was in place.
Both psychologists agreed on one thing immediately, stating that it would not benefit me to return to one-on-one home visits with mentally ill violent clients due to PTSD. These two client incidents also resulted in opening the door to past abuses, which I thought I had laid to rest with drugs, not phycological help. The real journey for mental health healing was now beginning.
Fortunately, I have a great psychologist who is walking with me during this journey. Once I was officially diagnosed with PTSD and depression, it was then that the hard emotional work began. Anxiety is also a part of PTSD. What may be worse is that my anger at those who refused to hear me when I adamantly spoke up about both clients’ dangerousness is overpowering. My words went ignored, and I feel like a lamb led to the lion’s den. My anger has affected how fast my recovery progresses.
Since both violent client episodes have thrown open the doors of PTSD and depression, I left the past traumas in a crack cocaine fog slithered back into my memories, setting fire to my anxiety. I had used crack cocaine to bury the sexual, physical, and emotional abuse I endured. The drugs hid the mental anguish I suffered as they slid to the farthest part of my mind. Only to wait for the first opportunity to reemerge.
Once placed in the firing line of assaults, the opportunity to the door of all things horrible made itself available. My mind became bombarded with a mixture of old and new traumas. Unable to unweave the torments and tortures of my mind without my old drug of choice, I welcomed the help of the professionals.
No matter how many drugs you do or much alcohol you drink, you cannot undo or erase the past. Interestingly, even as a mental health therapist, I knew I could not do therapy on myself. After all, I was now in the blurry bubble, not on the outside with objectivity. It would be best if I hung onto my sobriety.
I’ve been in therapy for ten months and still suffering from symptoms of PTSD, depression, and anxiety. Although I am in a better place than I was ten months ago, I know I still have work to do. I know for sure that I can no longer work with mentally ill clients at this time. It is not because they are mentally ill, but because of my flashbacks and my fear of being attacked, which is too intense and lacks employer support. To work with this population of people, you must have confidence and support. I’m not ready to go back and do not know if I will ever be able to return.
Without crack cocaine, this time, I was wide open to the signs of my mental health diagnosis. I am now working through trauma without my go-to solution. I am currently fighting my issues in the raw. These frightening, violent episodes with my clients were the first abuse issues I had to face in sobriety.
Without cocaine as my cover for pain, I felt like I was hanging in the wind. I became overtaken by emotional duress because of the assaults; however, even more so by the way the company I worked for handled both situations, leaving me out in the cold.
These last two incidents triggered nearly every sign of PTSD, depression, and anxiety to the max. I struggled daily, and after ten months of meeting with the psychologist, I still sometimes feel stuck in the symptoms. I believe that I hang onto them to keep me guarded for anything that may happen to me. Fear is not the right way to live.
Before the virus changed eating out in restaurants, I made it a point to face the doors. I struggled, knowing someone was sitting nearby my seat. I do not want people anywhere behind me. I don’t particularly appreciate someone catching me off guard unless invited into my space.
I do not trust my safety around people I do not know. I stay prepared for anything wrong to happen. I struggle with phone conversations with businesses because my mind wants to hear what I want to hear. I know I can be problematic to deal with over the phone.
I am on alert at all times, fearing another home invasion like the one that almost led to my murder nearly twenty years ago. My heart begins to pound if someone unexpectedly knocks on my door. If a car seems to be following me as I head home, I may drive past my street, so they don’t know where I live.
I have difficulty sleeping, and when I do, I often have frightening nightmares. A few weeks ago, I had a nightmare about being kidnapped. Once I realized I was still in my home, I walked to the bedroom deck to look outside. I noticed an unfamiliar white car parked in front of my house across the street. It was parked there all day. And I looked out of my window all day, fearing whoever was parked there was casing my home.
When depression rules the day, I might stay in bed until I have a reason not to. For a time, I stopped caring about how I looked and my daily hygiene. Every day I put on the same clothes unless I had a doctor’s appointment. On some days, I didn’t want to live, and one night I took some pills my back surgeon prescribed for pain. I guess I was lucky that the pills made me sick and eventually came back up. I started bingeing and purging daily. The only thing that did not change was keeping my sobriety. That is still important to me, perhaps one of the few items of importance at this time.
I believe my psychologist is correct about not seeing clients anymore. I am too paranoid. I filed grievances against my former company and TennCare insurance. Neither accepts what my feelings are about what happened to me. Neither is willing to accept any responsibility for what happened to me after voicing my concerns before the assaults. So, returning to this job for this type of job is no longer possible. It saddens me because I worked hard for my education to work in the mental health field. I loved my work.
Because of the October 2019 assault, I had to have my third back surgery in October 2020. That also increased my depression. I know part of my struggle moving forward with my mental health was my former supervisor’s decision to send me into homes that no other agencies would continue to engage with or return staff to after assaults of employees. I am so angry about that.
What I do know is that as a former therapist, I have sat with many clients who swore they were over their past traumas simply because they stopped thinking about it. Many are unable to realize how their past has affected their present and will affect their future. They will often state that they may have seen a therapist a few times or had taken medication for their PTSD and depression; however, not compliant with medical instructions. Yet, they sit in front of me crying as if the abuse they suffered just happened today and not twenty or more years ago.
Saying you are seeing a therapist and putting in the work to see a therapist are two different things. The same goes for taking medication; taking it and saying you are taking it is also two separate things. Although medicine is not always needed, meeting with a psychologist is significant. If medication is to be required, let the psychologist make that decision. Do not try to self-medicate on your own. Because it would only be temporary, it will not help you.
The results or consequences of traumatic events forever stay imprinted in the very depths of our minds and souls. They change how we live, survive, and see the world. Without realizing it, we also passed them on to our children, handicapping their personal growth and survival ability. Some people will freely tell others that they need to suck it up and move on; however, beatings, rapes, and seeing death hide away until it is time to show its horror. You will be unprepared for what happens next, and so will those who love you. PTSD does not go away; you learn how to control it and not let it control you.
Do not wait for the return of ugliness to reappear. Get help for yourself or someone you love as soon as the first signs of PTSD and depression emerge after distressing events occur. The longer it takes to get help, the longer it takes for recovery and support to help. Below are signs and symptoms to notice. Make an appointment with a mental health agency as soon as possible.
PTSD – Behavioral: agitation, irritability, hostility, hypervigilance, self-destructive behavior, or social isolation. Psychological: flashback, fear, severe anxiety, or mistrust. Mood: loss of interest or pleasure in activities, guilt, or loneliness. Sleep: insomnia or nightmares, emotional detachment, or unwanted thoughts.
Depression – Mood: anxiety, apathy, general discontent, guilt, hopelessness, loss of interest or pleasure in activities, mood swings, or sadness. Behavioral: agitation, excessive crying, irritability, restlessness, or social isolation. Sleep: early awakening, excess sleepiness, insomnia, or restless sleep. Whole-body: extreme hunger, fatigue, or loss of appetite. Cognitive: lack of concentration, slowness in activity, or thoughts of suicide. Weight: weight gain or weight loss, poor appetite, or repeatedly going over thoughts.
Anxiety – Behavioral: hypervigilance, irritability, or restlessness. Cognitive: lack of concentration, racing thoughts, or unwanted thoughts. Whole-body: fatigue or sweating, anxiety, excessive worry, fear, feeling of impending doom, insomnia, nausea, palpitations, or trembling.